Few interesting cases were seen in today's ward-round
1. A 60-year old lady who's previously well with only known hypertension was admitted with 1 month's history of progressive bilateral glove-stocking distribution of sensory loss, tingling pain, and proximal / distal muscle weakness. Examination showed wasting of small hand & feet muscles, power 3 in all 4 limbs, generalised hyporeflexia & hypotonia in all 4 limbs, CN VII / XII palsy, and mild bilateral ptosis. Otherwise, ECG, cardiovascular, GI, and urological symptoms were unable. Patient is currently investigated for nerve conduction abnormalities, and herself & family are uncertain about this thus deferred. Possible diagnosis include CIDP v.s. other causes of peripheral sensory-motor polyneuropathy
Reading:
- CIDP on emedicine
2. Found out from renal that statin-induced myopathy is more common in nephrotic syndrome. A young man in his mid-thirities was admitted for headache which turned out to be a cerebral sinus thrombosis. His cholesterol was noted to be very high thus recommended to increase his simvastatin to atorvastatin 80mg. Baseline LFT was normal, however his renal team came by and recommended his dose to be reduced because of increased rhabdomyolysis risk
- Further raeding on FDA
Saturday, May 10, 2008
Friday, May 9, 2008
The Lunatic Lament - Story of Syphilis
There was a young man of Back Bay
Who thought syphilis just went away.
And thought that a chancre
Was merely a canker
Acquired in lascivious play.
Now first he got acne vulgaris,
The kind that is rampant in Paris
It covered his skin
From forehead to shin
And now people ask where his hair is.
With symptoms increasing in number,
His aorta's in need of a plumber
His hear is cavorting
His wife is aborting
And now he's acquired a gumma.
Consider his terrible plight -
His eyes won't react to the light
His hands are apraxic.His gait is ataxic.
He's developing gun-barrel sight.
His passions are strong as before
But his penis is flaccid, and sore.
His wife now has tabes
And sabre-shinned babies
She's really worse off than a whore.
There are pains in his belly and knees.
His sphincters have gone by degrees.
Paroxysmal incontinence,
With all its concomitants,
Brings on quite unpredictable pees.
Though treated in every known way,
His spirochetes grow day by day.
He's developed paresis,
Converses with Jesus,
And thinks he's the Queen of the May."
By Isaac Asimov
This poetic manifest reveals the myriad of sickening phenomenon arising from this chronic, indolent infection.
Further reading:
1. Links to emedicine on neurosyphilis
Who thought syphilis just went away.
And thought that a chancre
Was merely a canker
Acquired in lascivious play.
Now first he got acne vulgaris,
The kind that is rampant in Paris
It covered his skin
From forehead to shin
And now people ask where his hair is.
With symptoms increasing in number,
His aorta's in need of a plumber
His hear is cavorting
His wife is aborting
And now he's acquired a gumma.
Consider his terrible plight -
His eyes won't react to the light
His hands are apraxic.His gait is ataxic.
He's developing gun-barrel sight.
His passions are strong as before
But his penis is flaccid, and sore.
His wife now has tabes
And sabre-shinned babies
She's really worse off than a whore.
There are pains in his belly and knees.
His sphincters have gone by degrees.
Paroxysmal incontinence,
With all its concomitants,
Brings on quite unpredictable pees.
Though treated in every known way,
His spirochetes grow day by day.
He's developed paresis,
Converses with Jesus,
And thinks he's the Queen of the May."
By Isaac Asimov
This poetic manifest reveals the myriad of sickening phenomenon arising from this chronic, indolent infection.
Further reading:
1. Links to emedicine on neurosyphilis
Simple approach to ABG interpretation
Have came across numerous ABG interpretation books, and so far this frame work provides the easiest & fastest application. Adopted from BMJ / TTSH Intensive care handbook.
Hope you may find this helpful too (note inter-personal preferences may vary)
Hope you may find this helpful too (note inter-personal preferences may vary)
Wednesday, May 7, 2008
Reading: Procalcitonin
Today I was asked to order procalcitonin test for a patient with suspected infection.
The patient was well, no particular localising symptoms currently. However approximately 2 weeks ago he was treated as probable meningoencephalitis with improvment of headache & diplopia. Lab results returned normal, and an informative lab message showed:
" Procalcitonin: +ve if elevated suggestive of bacterial / parasite / fungal infections. It may not be raised in localised infection, chronic inflammation, or chronic autoimmune diseases. It is not usually elevated in fracture / surgery, and rarely exceeds 5. Procalcitonin begins to rise after onset of infection in 2hrs, peaks in 12 - 24 hours, and 1/2 life 22 - 29 hours".
Attacked reference: wikipedia (inside contain reading links)
The patient was well, no particular localising symptoms currently. However approximately 2 weeks ago he was treated as probable meningoencephalitis with improvment of headache & diplopia. Lab results returned normal, and an informative lab message showed:
" Procalcitonin: +ve if elevated suggestive of bacterial / parasite / fungal infections. It may not be raised in localised infection, chronic inflammation, or chronic autoimmune diseases. It is not usually elevated in fracture / surgery, and rarely exceeds 5. Procalcitonin begins to rise after onset of infection in 2hrs, peaks in 12 - 24 hours, and 1/2 life 22 - 29 hours".
Attacked reference: wikipedia (inside contain reading links)
Monday, May 5, 2008
Mnemonics - Extensor plantars & absent ankle jerks (PG)
Sex can make those 'F***ing' ankles clutch down (From anonymous author)
Cauda equina lesion
Motor neuron disease
Tabes Dorsalis *syphilis*
Frideriech's ataxia
CVA + Diabetes
Menomoics - Autonomic Drugs
Anticholinergic drug side-effects:
"Know the ABCD's of anticholinergic side-effects"
- Anorexia
- Blurred vision
- Constipation / confusion
- Dry mouth / dilated pupils ('ANTI' constriction)
- Sedation / urinary stasis
Cholinergics - "IF you know these, you will be 'LESS DUMB'"
- Lacrimation
- Excitation of nicotinic receptors
- Salvation
- Sweating
- Diarrhoea
- Urination/micturition
- Broncho-constriction
* 'Con' stricts the pupil
"Know the ABCD's of anticholinergic side-effects"
- Anorexia
- Blurred vision
- Constipation / confusion
- Dry mouth / dilated pupils ('ANTI' constriction)
- Sedation / urinary stasis
Cholinergics - "IF you know these, you will be 'LESS DUMB'"
- Lacrimation
- Excitation of nicotinic receptors
- Salvation
- Sweating
- Diarrhoea
- Urination/micturition
- Broncho-constriction
* 'Con' stricts the pupil
Neurology reading of the week: GBS, CVA, Peripheral neuropathy
First day in neurology's encountered with few interesting cases:
- Stroke
- Guillain Barre Syndrome
- Peripheral neuropathy - secondary to amyloidosis
Please click on the links below
1. GBS on eMedicine: See my summarised sheet on google docs
2. Stroke (NEJM Review)
3. Peripheral neuropathy
- Stroke
- Guillain Barre Syndrome
- Peripheral neuropathy - secondary to amyloidosis
Please click on the links below
1. GBS on eMedicine: See my summarised sheet on google docs
2. Stroke (NEJM Review)
3. Peripheral neuropathy
Thursday, May 1, 2008
Presentation of the week - ECG changes in a poisoned patient
This week was asked to prepare a talk on ECG rounds. The topic that I chose was ECG changes in a poisoned patient. It is interesting to know how different drugs (especially anti-arrhythmics) can cause ECG changes and it can help us appreciate the myocardial electrophysiology.
Hope you'll find this helpful.
Hope you'll find this helpful.
Sunday, April 20, 2008
This Weeks' Reading
The important and interesting theme of this week is deficiency anaemias, something which is frequently encountered in almost any field of medical specialty.
For review:
1. Iron deficiency anaemia
2. B12 and folate deficiency anaemia
3. Interesting read: BMJ editorial on difficulty in distinguishing anaemia of chronic disease from other causes
For review:
1. Iron deficiency anaemia
2. B12 and folate deficiency anaemia
3. Interesting read: BMJ editorial on difficulty in distinguishing anaemia of chronic disease from other causes
Saturday, April 19, 2008
Summary sheet - Assessment of an acutely poisoned patient
Summary sheet - Polymyalgia Rheumatica

Polymyalgia is one of the most common inflammatory rheumatic disease characterised by pain and stiffness of proximal muscles (especially in the shoulder girdle) in elderly Caucasians and requires long-term treatment with glucocorticoids. There is strong relationship with giant cell arteritis.
This summary sheet provides a quick-glance format for key facts on PMR - its diagnosis, important differentials, and management methods which will be helpful for clinical practice and exam purposes.
Comments welcome.
Tuesday, April 15, 2008
Reading - Pulmonary Hypertension in Critical Care
Last week's reading was on pulmonary hypertension.
( Roham TZ et al. Managing strategies for patient with pulmonary hyertension in the ICU. Critical Care Medicine 2008)
This paper highlights that pulmonary hypertension and concomitant right ventricular failure present a particularly difficult diagnostic and therapeutic challenge in haemodynamically unstable patients in the ICU.
The categories of underlying aetiology can be sub-divided into those that causes:
1) pulmonary arterial hypertension;
2) associated with significant venous or capillary disease;
3) secondary to left heart disease;
4) Due to lung disease or hypoxaemia
5) due to thrombotic / embolic diseases
There are few important learning messages from this paper:
1) Fluid resuscitation must be carefully initiated because intravascular depletion (hence low pre-load) or over-load can worsen haemodynamics.
2) Mechanical ventilation - especially at high tidal volume and high PEEP can worsen pulmonary hypertension and hence haemodynamics (Target PEEP 5 - 8).
3) Effective treatment relies on ability to accurately identify the underlying cause - from history, thorough examination, and appropriate investigations (ECHO; the gold-standard cardiac catheterisatio; ECG, CXR etc) and address the primary cause.
4) Although studies of inotropes and vasodilators in pulmonary hypertension (especially in ICU) are limited, the use of dobutamine, inhaled nitric oxide, and IV prostacycline have the greatest support in the literature). As for other treatments, relies on good understanding of their pharmacokinetics / dynamics and co-morbidities of the patient being treated.
5) The use of vasopressors should be carefully titrated to their lowest effective dose due to higher risk of side-effects without extra treatment benefits. Such important side-effects include tachycardia, increasing cardiac oxygen demand, profound hypotension, and arrhythmias.
( Roham TZ et al. Managing strategies for patient with pulmonary hyertension in the ICU. Critical Care Medicine 2008)
This paper highlights that pulmonary hypertension and concomitant right ventricular failure present a particularly difficult diagnostic and therapeutic challenge in haemodynamically unstable patients in the ICU.
The categories of underlying aetiology can be sub-divided into those that causes:
1) pulmonary arterial hypertension;
2) associated with significant venous or capillary disease;
3) secondary to left heart disease;
4) Due to lung disease or hypoxaemia
5) due to thrombotic / embolic diseases
There are few important learning messages from this paper:
1) Fluid resuscitation must be carefully initiated because intravascular depletion (hence low pre-load) or over-load can worsen haemodynamics.
2) Mechanical ventilation - especially at high tidal volume and high PEEP can worsen pulmonary hypertension and hence haemodynamics (Target PEEP 5 - 8).
3) Effective treatment relies on ability to accurately identify the underlying cause - from history, thorough examination, and appropriate investigations (ECHO; the gold-standard cardiac catheterisatio; ECG, CXR etc) and address the primary cause.
4) Although studies of inotropes and vasodilators in pulmonary hypertension (especially in ICU) are limited, the use of dobutamine, inhaled nitric oxide, and IV prostacycline have the greatest support in the literature). As for other treatments, relies on good understanding of their pharmacokinetics / dynamics and co-morbidities of the patient being treated.
5) The use of vasopressors should be carefully titrated to their lowest effective dose due to higher risk of side-effects without extra treatment benefits. Such important side-effects include tachycardia, increasing cardiac oxygen demand, profound hypotension, and arrhythmias.
Saturday, April 12, 2008
New summary sheet - pulsus paradoxus de-mysti-fied
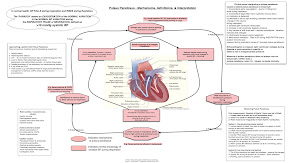
Been experimenting with my mac's OmniGraffle for building diagrams.
I'm highly impressed with this software's user-friendliness & graphics interface.
Please feel free to have a read, hope you'll find this useful.
Comments welcome!
(Please click my summary sheets column on the right side for more slides)
Wednesday, April 9, 2008
Ward round 9 Apr 2008 - Ischaemic Colitis
The disease of this week is ischaemic colitis. It is sometimes a challenging disease for physicians to make a correct diagnosis and initiate the definitive treatment - yes, is to transfer the patient to the surgeons STAT.
Textbooks describe the classical features of extremely severe abdominal pain out of proportion with physical examination findings. However patient (especially the elderly, long-standing diabetics) may present with vague or atypical symptoms, and may not mount any inflammatory or febrile response (typically raised CRP, fever). Sometimes may be a patient with long-standing atrial fibrillation or vascular disease who suddenly deteriorates.
My first patient was a gentleman who was admitted to cardiology from A&E for preliminary diagnosis of fast atrial fibrillation & acute pulmonary oedema. His past medical history consists of long-standing diabetes mellitus type II complicated by neuropathy & nephropathy, hypertension, hyperlipidaemia, ischaemic heart disease underwent a bypass many years ago, and chronic atrial fibrillation on warfarin treatment but very good INR control. He has been well otherwise & compliant with his medications until the week before admission when he started to complain of increasing fatigue, breathlessness, and reduced appetite due to a vague 'uncomfortable & sinking feeling' down his lower abdomen. He was haemodynamically stable and afebrile, but breathless at rest with respiratory rate 26 per minute, saturatioin 98% breathing 50% oxygen. Abdominal examination found only mild right upper quadrant and epigastric pain.
His haematology & glucose investigations were unremarkable, however his biochemistry revealed unexplained severe high-anion gap metabolic acidosis, renal & liver failure with markedly raised ALT, AST, Bil, CK, Cr, and mildly raised amylase. It is highly unusual to find such abnormal results in patients purely with cardiac or pulmonary diseases, and we must suspect other underlying causes. Indeed, cardiac enzymes in series showed no rising trend. He was given IV maintenance fluids and empirical antibiotics for possible sepsis. The on-call surgeons were informed to evaluate our patient for suspected acute abdomen especially ischaemic colitis. CT with contrast subsequently confirmed the diagnosis of multiple infarcts in the colon and kidneys. He was sent for urgent laparotomy.
Learning points:
1. Early diagnosis of ischaemic colitis in a patient with severe metabolic acidosis.
2. Ischaemic colitis on emedicine
Textbooks describe the classical features of extremely severe abdominal pain out of proportion with physical examination findings. However patient (especially the elderly, long-standing diabetics) may present with vague or atypical symptoms, and may not mount any inflammatory or febrile response (typically raised CRP, fever). Sometimes may be a patient with long-standing atrial fibrillation or vascular disease who suddenly deteriorates.
My first patient was a gentleman who was admitted to cardiology from A&E for preliminary diagnosis of fast atrial fibrillation & acute pulmonary oedema. His past medical history consists of long-standing diabetes mellitus type II complicated by neuropathy & nephropathy, hypertension, hyperlipidaemia, ischaemic heart disease underwent a bypass many years ago, and chronic atrial fibrillation on warfarin treatment but very good INR control. He has been well otherwise & compliant with his medications until the week before admission when he started to complain of increasing fatigue, breathlessness, and reduced appetite due to a vague 'uncomfortable & sinking feeling' down his lower abdomen. He was haemodynamically stable and afebrile, but breathless at rest with respiratory rate 26 per minute, saturatioin 98% breathing 50% oxygen. Abdominal examination found only mild right upper quadrant and epigastric pain.
His haematology & glucose investigations were unremarkable, however his biochemistry revealed unexplained severe high-anion gap metabolic acidosis, renal & liver failure with markedly raised ALT, AST, Bil, CK, Cr, and mildly raised amylase. It is highly unusual to find such abnormal results in patients purely with cardiac or pulmonary diseases, and we must suspect other underlying causes. Indeed, cardiac enzymes in series showed no rising trend. He was given IV maintenance fluids and empirical antibiotics for possible sepsis. The on-call surgeons were informed to evaluate our patient for suspected acute abdomen especially ischaemic colitis. CT with contrast subsequently confirmed the diagnosis of multiple infarcts in the colon and kidneys. He was sent for urgent laparotomy.
Learning points:
- Suspect fatal ischaemic colitis in the differential diagnosis of abdominal pain - especially in the context of patients with high risk factors.
- Cardiac or pulmonary diseases frequently present with 'abdominal discomfort' and may be difficult to distinguish from acute abdominal disease processes.
- Severe ischaemic colitis may manifest atypically with minimal abdominal findings.
- Clinicians should have a low threshold of suspicion for ischaemic bowel in patients with unexplained severe metabolic acidosis.
1. Early diagnosis of ischaemic colitis in a patient with severe metabolic acidosis.
2. Ischaemic colitis on emedicine
Monday, April 7, 2008
Best wishes for JM's trip to Delhi for his MRCS exams!

He will be leaving from 14 - 21 Apr for his exams, please wish him best of luck!
Please take this moment to read up a few things about Delhi:
1. Malarial prophylaxis2. FCO information for travelers (India)
3. About Delhi (Lonely Planet)
4. CDC's traveler's health (India)
Interesting readings for next week (Theme: Critical care medicine)
Pulsus Paradoxus (Plus how to measure properly!!)
Management of pulmonary hypertension in critical care
Management of delirium in the ICU and a good quick summary sheet published by its authors
which highlights the diagnosis of delirium requiers
1) acute onset of fluctuating altered mental status &
2) inattention
PLUS
3) disorganised thinking OR 4) Altered level of consciousness.
Homework: please summarise the KEY points each topic to no more than 1 A4 sheet, or 7 minutes short presentation.
Sunday, April 6, 2008
Good luck and have a smooooth MRCP exam for all candidates!
The blog master's currently out of service
Be back after examination's over
Wish me (all everyone of you) luck!
Be back after examination's over
Wish me (all everyone of you) luck!
Subscribe to:
Posts (Atom)

