The important and interesting theme of this week is deficiency anaemias, something which is frequently encountered in almost any field of medical specialty.
For review:
1. Iron deficiency anaemia
2. B12 and folate deficiency anaemia
3. Interesting read: BMJ editorial on difficulty in distinguishing anaemia of chronic disease from other causes
Sunday, April 20, 2008
Saturday, April 19, 2008
Summary sheet - Assessment of an acutely poisoned patient
Summary sheet - Polymyalgia Rheumatica

Polymyalgia is one of the most common inflammatory rheumatic disease characterised by pain and stiffness of proximal muscles (especially in the shoulder girdle) in elderly Caucasians and requires long-term treatment with glucocorticoids. There is strong relationship with giant cell arteritis.
This summary sheet provides a quick-glance format for key facts on PMR - its diagnosis, important differentials, and management methods which will be helpful for clinical practice and exam purposes.
Comments welcome.
Tuesday, April 15, 2008
Reading - Pulmonary Hypertension in Critical Care
Last week's reading was on pulmonary hypertension.
( Roham TZ et al. Managing strategies for patient with pulmonary hyertension in the ICU. Critical Care Medicine 2008)
This paper highlights that pulmonary hypertension and concomitant right ventricular failure present a particularly difficult diagnostic and therapeutic challenge in haemodynamically unstable patients in the ICU.
The categories of underlying aetiology can be sub-divided into those that causes:
1) pulmonary arterial hypertension;
2) associated with significant venous or capillary disease;
3) secondary to left heart disease;
4) Due to lung disease or hypoxaemia
5) due to thrombotic / embolic diseases
There are few important learning messages from this paper:
1) Fluid resuscitation must be carefully initiated because intravascular depletion (hence low pre-load) or over-load can worsen haemodynamics.
2) Mechanical ventilation - especially at high tidal volume and high PEEP can worsen pulmonary hypertension and hence haemodynamics (Target PEEP 5 - 8).
3) Effective treatment relies on ability to accurately identify the underlying cause - from history, thorough examination, and appropriate investigations (ECHO; the gold-standard cardiac catheterisatio; ECG, CXR etc) and address the primary cause.
4) Although studies of inotropes and vasodilators in pulmonary hypertension (especially in ICU) are limited, the use of dobutamine, inhaled nitric oxide, and IV prostacycline have the greatest support in the literature). As for other treatments, relies on good understanding of their pharmacokinetics / dynamics and co-morbidities of the patient being treated.
5) The use of vasopressors should be carefully titrated to their lowest effective dose due to higher risk of side-effects without extra treatment benefits. Such important side-effects include tachycardia, increasing cardiac oxygen demand, profound hypotension, and arrhythmias.
( Roham TZ et al. Managing strategies for patient with pulmonary hyertension in the ICU. Critical Care Medicine 2008)
This paper highlights that pulmonary hypertension and concomitant right ventricular failure present a particularly difficult diagnostic and therapeutic challenge in haemodynamically unstable patients in the ICU.
The categories of underlying aetiology can be sub-divided into those that causes:
1) pulmonary arterial hypertension;
2) associated with significant venous or capillary disease;
3) secondary to left heart disease;
4) Due to lung disease or hypoxaemia
5) due to thrombotic / embolic diseases
There are few important learning messages from this paper:
1) Fluid resuscitation must be carefully initiated because intravascular depletion (hence low pre-load) or over-load can worsen haemodynamics.
2) Mechanical ventilation - especially at high tidal volume and high PEEP can worsen pulmonary hypertension and hence haemodynamics (Target PEEP 5 - 8).
3) Effective treatment relies on ability to accurately identify the underlying cause - from history, thorough examination, and appropriate investigations (ECHO; the gold-standard cardiac catheterisatio; ECG, CXR etc) and address the primary cause.
4) Although studies of inotropes and vasodilators in pulmonary hypertension (especially in ICU) are limited, the use of dobutamine, inhaled nitric oxide, and IV prostacycline have the greatest support in the literature). As for other treatments, relies on good understanding of their pharmacokinetics / dynamics and co-morbidities of the patient being treated.
5) The use of vasopressors should be carefully titrated to their lowest effective dose due to higher risk of side-effects without extra treatment benefits. Such important side-effects include tachycardia, increasing cardiac oxygen demand, profound hypotension, and arrhythmias.
Saturday, April 12, 2008
New summary sheet - pulsus paradoxus de-mysti-fied
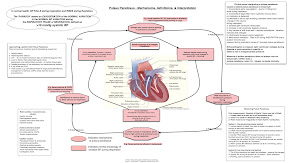
Been experimenting with my mac's OmniGraffle for building diagrams.
I'm highly impressed with this software's user-friendliness & graphics interface.
Please feel free to have a read, hope you'll find this useful.
Comments welcome!
(Please click my summary sheets column on the right side for more slides)
Wednesday, April 9, 2008
Ward round 9 Apr 2008 - Ischaemic Colitis
The disease of this week is ischaemic colitis. It is sometimes a challenging disease for physicians to make a correct diagnosis and initiate the definitive treatment - yes, is to transfer the patient to the surgeons STAT.
Textbooks describe the classical features of extremely severe abdominal pain out of proportion with physical examination findings. However patient (especially the elderly, long-standing diabetics) may present with vague or atypical symptoms, and may not mount any inflammatory or febrile response (typically raised CRP, fever). Sometimes may be a patient with long-standing atrial fibrillation or vascular disease who suddenly deteriorates.
My first patient was a gentleman who was admitted to cardiology from A&E for preliminary diagnosis of fast atrial fibrillation & acute pulmonary oedema. His past medical history consists of long-standing diabetes mellitus type II complicated by neuropathy & nephropathy, hypertension, hyperlipidaemia, ischaemic heart disease underwent a bypass many years ago, and chronic atrial fibrillation on warfarin treatment but very good INR control. He has been well otherwise & compliant with his medications until the week before admission when he started to complain of increasing fatigue, breathlessness, and reduced appetite due to a vague 'uncomfortable & sinking feeling' down his lower abdomen. He was haemodynamically stable and afebrile, but breathless at rest with respiratory rate 26 per minute, saturatioin 98% breathing 50% oxygen. Abdominal examination found only mild right upper quadrant and epigastric pain.
His haematology & glucose investigations were unremarkable, however his biochemistry revealed unexplained severe high-anion gap metabolic acidosis, renal & liver failure with markedly raised ALT, AST, Bil, CK, Cr, and mildly raised amylase. It is highly unusual to find such abnormal results in patients purely with cardiac or pulmonary diseases, and we must suspect other underlying causes. Indeed, cardiac enzymes in series showed no rising trend. He was given IV maintenance fluids and empirical antibiotics for possible sepsis. The on-call surgeons were informed to evaluate our patient for suspected acute abdomen especially ischaemic colitis. CT with contrast subsequently confirmed the diagnosis of multiple infarcts in the colon and kidneys. He was sent for urgent laparotomy.
Learning points:
1. Early diagnosis of ischaemic colitis in a patient with severe metabolic acidosis.
2. Ischaemic colitis on emedicine
Textbooks describe the classical features of extremely severe abdominal pain out of proportion with physical examination findings. However patient (especially the elderly, long-standing diabetics) may present with vague or atypical symptoms, and may not mount any inflammatory or febrile response (typically raised CRP, fever). Sometimes may be a patient with long-standing atrial fibrillation or vascular disease who suddenly deteriorates.
My first patient was a gentleman who was admitted to cardiology from A&E for preliminary diagnosis of fast atrial fibrillation & acute pulmonary oedema. His past medical history consists of long-standing diabetes mellitus type II complicated by neuropathy & nephropathy, hypertension, hyperlipidaemia, ischaemic heart disease underwent a bypass many years ago, and chronic atrial fibrillation on warfarin treatment but very good INR control. He has been well otherwise & compliant with his medications until the week before admission when he started to complain of increasing fatigue, breathlessness, and reduced appetite due to a vague 'uncomfortable & sinking feeling' down his lower abdomen. He was haemodynamically stable and afebrile, but breathless at rest with respiratory rate 26 per minute, saturatioin 98% breathing 50% oxygen. Abdominal examination found only mild right upper quadrant and epigastric pain.
His haematology & glucose investigations were unremarkable, however his biochemistry revealed unexplained severe high-anion gap metabolic acidosis, renal & liver failure with markedly raised ALT, AST, Bil, CK, Cr, and mildly raised amylase. It is highly unusual to find such abnormal results in patients purely with cardiac or pulmonary diseases, and we must suspect other underlying causes. Indeed, cardiac enzymes in series showed no rising trend. He was given IV maintenance fluids and empirical antibiotics for possible sepsis. The on-call surgeons were informed to evaluate our patient for suspected acute abdomen especially ischaemic colitis. CT with contrast subsequently confirmed the diagnosis of multiple infarcts in the colon and kidneys. He was sent for urgent laparotomy.
Learning points:
- Suspect fatal ischaemic colitis in the differential diagnosis of abdominal pain - especially in the context of patients with high risk factors.
- Cardiac or pulmonary diseases frequently present with 'abdominal discomfort' and may be difficult to distinguish from acute abdominal disease processes.
- Severe ischaemic colitis may manifest atypically with minimal abdominal findings.
- Clinicians should have a low threshold of suspicion for ischaemic bowel in patients with unexplained severe metabolic acidosis.
1. Early diagnosis of ischaemic colitis in a patient with severe metabolic acidosis.
2. Ischaemic colitis on emedicine
Monday, April 7, 2008
Best wishes for JM's trip to Delhi for his MRCS exams!

He will be leaving from 14 - 21 Apr for his exams, please wish him best of luck!
Please take this moment to read up a few things about Delhi:
1. Malarial prophylaxis2. FCO information for travelers (India)
3. About Delhi (Lonely Planet)
4. CDC's traveler's health (India)
Interesting readings for next week (Theme: Critical care medicine)
Pulsus Paradoxus (Plus how to measure properly!!)
Management of pulmonary hypertension in critical care
Management of delirium in the ICU and a good quick summary sheet published by its authors
which highlights the diagnosis of delirium requiers
1) acute onset of fluctuating altered mental status &
2) inattention
PLUS
3) disorganised thinking OR 4) Altered level of consciousness.
Homework: please summarise the KEY points each topic to no more than 1 A4 sheet, or 7 minutes short presentation.
Sunday, April 6, 2008
Good luck and have a smooooth MRCP exam for all candidates!
The blog master's currently out of service
Be back after examination's over
Wish me (all everyone of you) luck!
Be back after examination's over
Wish me (all everyone of you) luck!
Subscribe to:
Posts (Atom)

